6 Signs and Symptoms of Pancreatic Cancer
Pancreatic cancer is often called a “silent killer” because it tends to hide in the early stages. By the time symptoms show up, it’s sometimes already advanced.
But that doesn’t mean there aren’t warning signs—it just means we need to listen carefully.
Today, let’s talk about six important symptoms that may point to pancreatic cancer.
On their own, these signs could have other explanations—but when they persist or appear together, they deserve attention.
Number 6 – Unexplained Weight Loss
Sudden, unintentional weight loss is one of the most common symptoms of pancreatic cancer. You’re not dieting, you’re not exercising more, and yet the pounds are falling off.
Why? Because as the tumor grows, it can affect digestion and nutrient absorption. It might also signal that your body is burning more energy to fight the disease. If you’ve lost 10 pounds or more without trying—and especially if it happens quickly—it’s something worth checking out.
Number 5 – Upper Abdominal Pain or Back Pain
Pain that starts in the upper abdomen and radiates to the back can be a subtle but serious symptom. It often feels dull and persistent, and it may come and go at first.
This happens because the pancreas sits deep in the abdomen, near the spine and many nerves. As a tumor grows, it can press on these areas, triggering discomfort. Many people mistake it for muscle strain or even indigestion, which is why it’s so easy to overlook.
Number 4 – Jaundice (Yellowing of the Skin or Eyes)
Jaundice is a red flag—and it’s often one of the first visible signs of pancreatic cancer, especially when the tumor is near the head of the pancreas.
You might notice yellowing of the skin or the whites of the eyes, along with dark urine or pale stools. This happens because the tumor can block the bile duct, preventing bile from flowing properly out of the liver. The buildup of bilirubin in the body causes the yellowing.
If you ever see jaundice, don’t wait—it always needs to be evaluated promptly, even if it turns out to be something less serious.
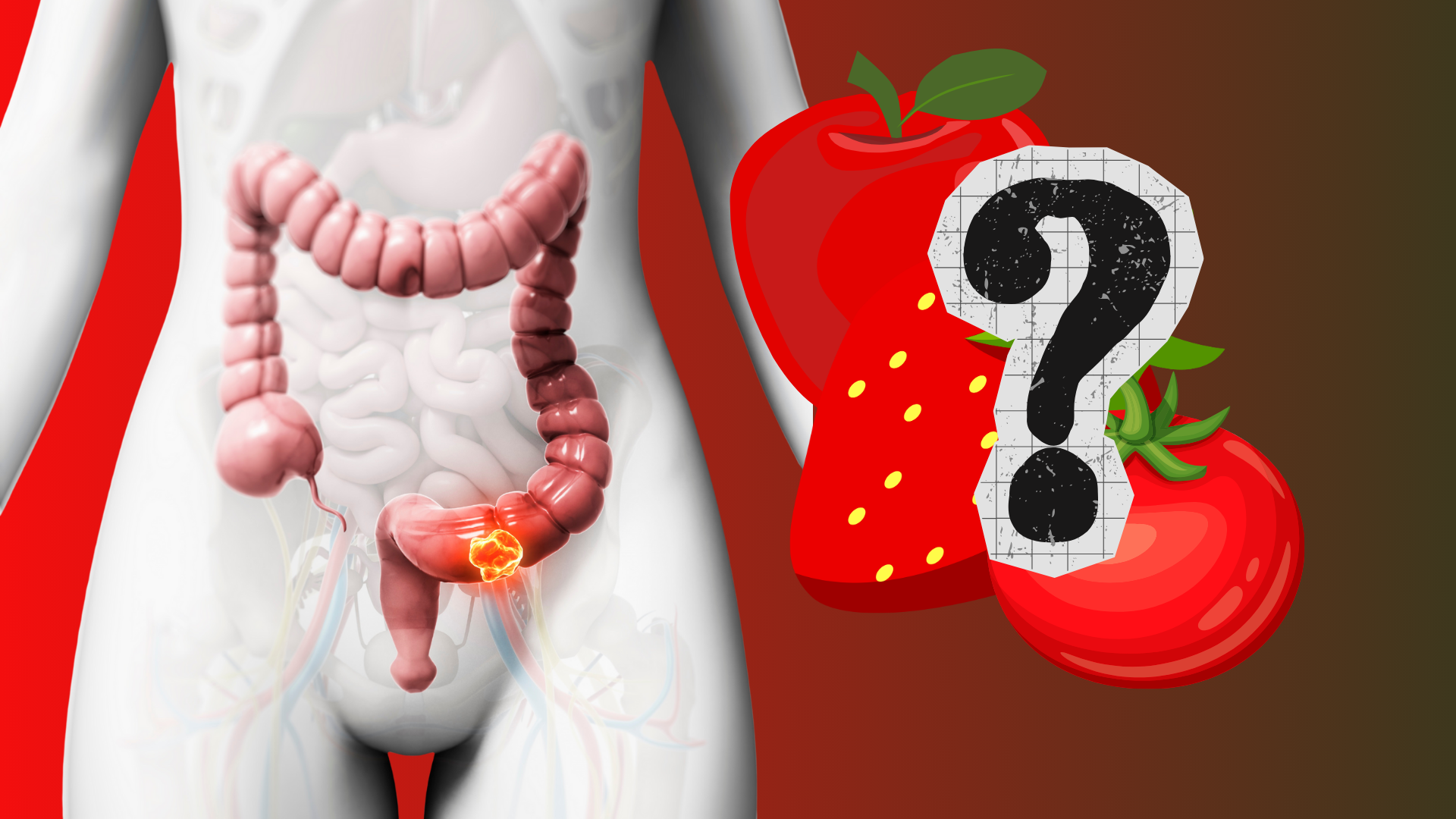
Number 3 – Changes in Stool or Digestion
Pancreatic cancer can interfere with the enzymes needed for digestion. That means your body might not break down fat properly, leading to greasy, pale, or floating stools. Some people also experience frequent bloating, nausea, or a feeling of fullness even after small meals.
If you notice ongoing digestive issues that don’t improve with dietary changes—or your bowel habits have changed significantly—this could be a sign that the pancreas isn’t functioning as it should.
Number 2 – New-Onset Diabetes or Blood Sugar Spikes
This one often surprises people. The pancreas is responsible for insulin production, so when it’s under attack, blood sugar regulation can be affected.
Some people are diagnosed with type 2 diabetes seemingly out of the blue—especially older adults with no family history or weight issues. Others notice high blood sugar, fatigue, or increased thirst. If diabetes comes on suddenly and doesn’t seem to fit the usual pattern, doctors may investigate pancreatic function more closely.
Number 1 – Fatigue and Weakness That Won’t Go Away
This is one of the most common symptoms across all types of cancer, but it’s still important. When your body is fighting something serious, it pulls energy away from daily functions. Add in the effects of poor digestion, possible anemia, and inflammation, and you’re left with persistent tiredness that sleep doesn’t fix.
If you’re feeling drained every day—especially in combination with weight loss or digestive issues—it’s time to listen to your body.
Who’s Most at Risk for Pancreatic Cancer?
Pancreatic cancer can happen to anyone, but some people are more vulnerable than others. Age is a major factor—most cases occur in people over 60, and it’s slightly more common in men.
Smoking is one of the biggest controllable risk factors. Long-term tobacco use can double your risk. People with chronic pancreatitis, a family history of pancreatic cancer, or certain genetic conditions—like BRCA2 mutations or Lynch syndrome—may also be more likely to develop it.
Even having long-standing type 2 diabetes or being significantly overweight can increase your risk. And while not everyone with these risk factors will get pancreatic cancer, knowing your personal risk can help guide more informed decisions about screening and monitoring.
Can Diet and Lifestyle Make a Difference?
There’s no guaranteed way to prevent pancreatic cancer—but your daily habits still matter. Diets high in red meat, processed foods, and added sugars have been associated with higher risk. On the other hand, eating more vegetables, fruits, whole grains, and healthy fats may support better pancreatic and digestive health.
Regular physical activity helps regulate insulin levels and reduce inflammation. And if you smoke, quitting is one of the most important steps you can take—not just for your pancreas, but for your overall cancer risk.
Reducing alcohol intake may also help, as heavy alcohol use can contribute to pancreatitis, which in turn increases the risk of cancer.
Taking care of your pancreas doesn’t require perfection—just consistency and balance.
So What Should You Do?
Most of these symptoms can be caused by other conditions. But the key is persistence. If you’ve had any of these signs for several weeks—and they’re not improving—it’s worth a conversation with your doctor.
Early detection of pancreatic cancer is challenging, but not impossible. And spotting the warning signs early is still our best defense.